
Most people do not see the potential danger in the appearance of small epithelial tumors in the body, but papillomas are not just a cosmetic defect. In some cases they can have irreversible consequences. The growths appear as a result of infection with HPV, a highly contagious virus that has more than 100 genotypes and some of its types can cause the development of oncological processes. It is easy to become infected with HPV, so to avoid infection it is important to know how HPV is transmitted and what factors contribute to the spread of virions.
All routes of HPV infection
There is a tendency that in families where there is a carrier of the virus, in 50-70% of cases the people around him become infected. The main danger is that the infection, upon entering the body, does not manifest itself immediately, so a person may not learn about the infection for a long time and continue to be in close contact with relatives.
Important!
The absence of external manifestations of HPV does not guarantee that an infected person is absolutely safe for his close circle.
Household contact infection
A virus carrier can transmit a pathogenic virion (viral particle) to a healthy person through:
- Ordinary tactile contact, for example, hugs, handshakes. The likelihood of contracting HPV increases if there are lesions on the skin (even small wounds, abrasions or scratches are enough for the infection to penetrate a healthy body);
- Using personal objects of a sick person. Viral particles can live for a long time on bedding, towels, underwear, cloths and other everyday products;
- While kissing. HPV DNA is not only found in the epithelium, but is present in all the biological fluids of an infected person and can therefore be transmitted through saliva during a kiss.
Additionally, one can become infected with HPV by visiting public places such as saunas, swimming pools or gyms, where there are large crowds of people, many of whom neglect basic protection rules. Therefore, it is necessary to use exclusively personal and household hygiene products.
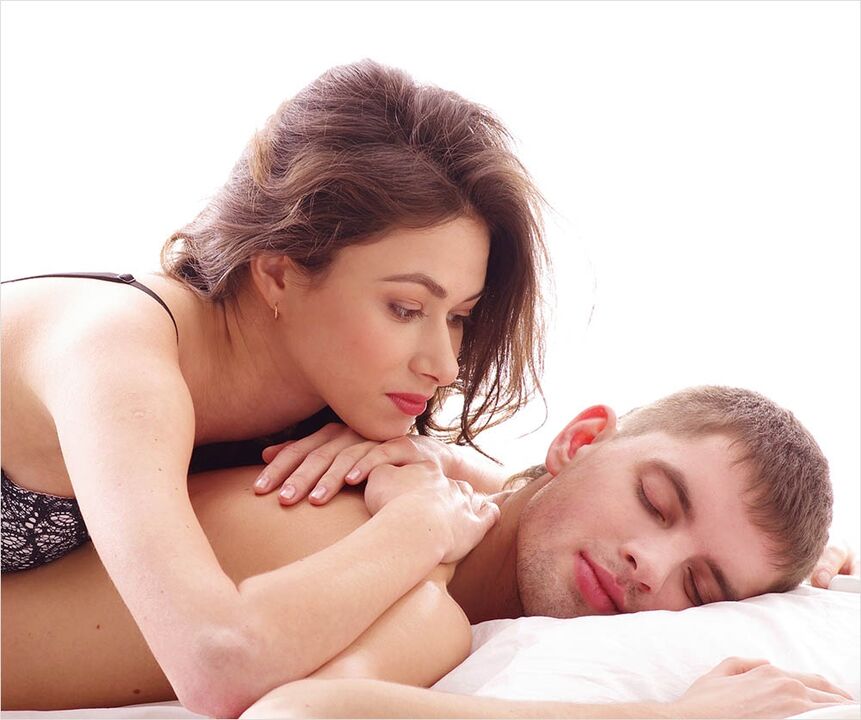
Sexual transmission of the virus.
The most common route of transmission of human papillomavirus infection is through sexual contact. If a partner, whether male or female, is a carrier of the virus, it is enough to have sexual intercourse once to become infected with HPV (infection occurs in 95% of cases).
The virus is transmitted through any type of sexual interaction, whether oral, vaginal or anal, while the presence of condylomas in the anogenital area of the partner increases the risk of infection by up to 100%.
It is interesting that not even a condom can completely protect against possible infection:
- First of all, papillomatous rashes can be localized not only on the genitals, but also in the groin and anus. Therefore, upon contact with unprotected areas of the body, the virus can easily be transmitted from one partner to another;
- Secondly, the latex that the condom is made of has quite large pores. Viral particles penetrate through them without obstacles.
Infection with oncogenically dangerous types of papillomaviruses occurs mainly during sexual contact. If the carcinogenic type of HPV is transmitted to women, they develop a neoplasm that can become cervical cancer.
Despite the fact that oncological pathologies of the genital organs are less common in men, the presence of genital papillomas increases the risk of malignancy. If infection with a carcinogenic virus occurs during oral sex, the likelihood of developing tonsil cancer increases.
Vertical infection (from mother to child)
Children can become infected with the papillomavirus in the womb or immediately at birth (during passage through the natural birth canal). Additionally, if the mother's HPV progresses (is in the active phase), the baby's risk of infection increases.

Intrauterine infection is extremely rare, since the placenta can protect the embryo from many pathogenic factors, including viral infections. Cases of HPV transmission to a baby during passage through the birth canal of an infected mother are recorded more frequently.
At the time of birth, the mucous membranes of the child's larynx and trachea are affected, which subsequently leads to recurrent respiratory papillomatosis (RRP). This is a dangerous pathology that poses a threat to the baby's life. Over the course of 1 to 2 years, children with RRP develop benign neoplasms of the trachea and larynx, which block the airways and cause suffocation.
In such a situation, only surgical removal of papillomatous growths will help; However, even after destruction, tumors usually reappear. Parents whose children suffer from PRR should carefully monitor the state of their immune system, since decreased immunity increases the risk of relapse.
Some women preparing to become mothers worry that the child could inherit the papillomavirus, but this is not the case. The routes of infection are described above, the hereditary factor is completely excluded: HPV is a virus that is not transmitted genetically.
Autoinoculation infection method.
Autoinfection (autoinoculation) is a fairly common type of infection. An infected person should understand that any trauma to tumors can cause additional growths to form.
Papillomas located on the face, neck, armpits or groin are often cut with a razor, scratched or torn during hygiene procedures. When the integrity of growth is disturbed, blood escapes and flows to neighboring healthy areas of the body. Since viral particles are present in all biological fluids of the patient, blood entering the clean epithelium causes the spread of infection and the formation of multiple papillomatous rashes.
In addition, scratching the growths with your nails leaves particles of pathogenic epithelium under the plaques, which often also contributes to autoinfection. For example, after a person has scratched a papilloma with his nails and suddenly decides to scratch his ear or nose, if there is the slightest damage to the epithelium, the virus will definitely "settle" in it and then manifest itself . as characteristic growths.

After its introduction into the body, HPV activation is not immediately observed; The virus requires certain conditions for its full functioning.
When and what triggers HPV activation
How quickly and actively the papillomavirus begins to behave after infection is determined by the immune status of the infected person. HPV is part of the group of immune-dependent viruses, so it is during a decrease in immune defenses that its activation occurs.
The body of a healthy person, even after infection, is capable of producing a sufficient number of antibodies to completely resist viral attacks. In these people, the disease progresses latently (in latent mode), so epithelial tumors do not appear in the body.
When the immune system is weakened, it produces significantly fewer antibodies that cannot suppress the virus on their own, and then HPV is activated with the formation of a papillomatous rash. The following unfavorable factors can provoke the transition of the papillomavirus to the active phase:
- any pathology of an infectious nature recently suffered;
- long-term use of oral contraceptives;
- uncontrolled use of cytostatic drugs (suppress the immune system);
- dysfunction in the endocrine system;
- pathological condition of the gastrointestinal tract, in particular intestinal dysbiosis;
- psychoemotional disorders associated with frequent stress, nervousness, fatigue;
- helminth infestations;
- frequent inflammatory skin diseases;
- presence of bad habits (smoking, drinking alcohol, drugs).
Important!
Any factor that reduces the effectiveness of the human immune system can lead to HPV activation.
The formation of the first growths is a reason to consult a doctor. It is not necessary to self-medicate, since in some cases inadequate therapy for papillomas leads to the development of cancerous tumors.
Papillomavirus treatment
Since no drugs have yet been invented that can cure the papillomavirus, it is impossible to completely eliminate it from a person's body after the age of 30. Cases of HPV elimination are only recorded in young people under 25 years of age.
Treatment of papillomatosis is carried out in three directions:
- suppression of viral activity (returning it to a latent state) when taking antiviral drugs;
- increase the patient's immune status through the use of drugs with interferon;
- destruction of pathological neoplasms using minimally invasive hardware techniques;
- Cytostatic drugs are prescribed when there is a high probability of malignancy of papillomas (they disrupt the division process of atypical cells).
Antiviral medications prescribed by a doctor may be for oral, topical, injectable, or rectal use:

- Tablets (oral use);
- Gels, ointments (external use);
- Injections (injections);
- Suppositories (rectal suppositories).
Immunomodulatory drugs can also be prescribed in different forms, most often these are tablets and gels for the external treatment of tumors.
Cytostatics are prescribed if, after diagnosis, it is determined that the papillomatous rashes are caused by a highly oncogenic type of HPV.
The most frequently used destructive techniques to remove pathological tumors are:
- Electrocoagulation– cauterization of growths with electric current. The procedure is painful and leaves visible scars;
- cryotherapy– the papilloma freezes under the influence of liquid nitrogen, leaving no traces, but the procedure is recommended to remove small superficial tumors;
- laser destruction– suitable for removing superficial and deep papillomas, a good cosmetic effect allows it to be used on open parts of the body;
- radio wave technique– The removal of growths is carried out without contact, with a short recovery period, there are no traces or scars left after the intervention.
After completing the course of treatment, do not forget about preventive medical examinations. It is necessary to carry out regular tests (preferably every year) for HPV, and also carefully monitor the state of the immune system.















